A Prevalent Condition with Limited Solutions
Overactive bladder (OAB) affects over 546 million people worldwide, often leading to sudden urgency, involuntary leakage, and frequent daytime and nighttime urination. While awareness is increasing—driven by aging populations and improved diagnostics—current therapies remain limited by side effects, inconsistent results, and high patient dropout rates. There is a clear clinical need for a more targeted, effective solution.
The Challenge
Conventional treatment options for OAB include oral anticholinergic medications, botulinum toxin injections, neuromodulation, and tibial nerve stimulation. However, each presents significant limitations. Medications often cause intolerable side effects, resulting in more than 80% of patients discontinuing use within the first year. Botox injections are generally administered without precise targeting, which can lead to complications such as urinary retention. Neuromodulation and nerve stimulation treatments show variable success rates—often below 50%—and typically require repeated clinic visits. A key challenge in improving outcomes is the inability to identify and treat the precise areas of bladder overactivity.
The Solution
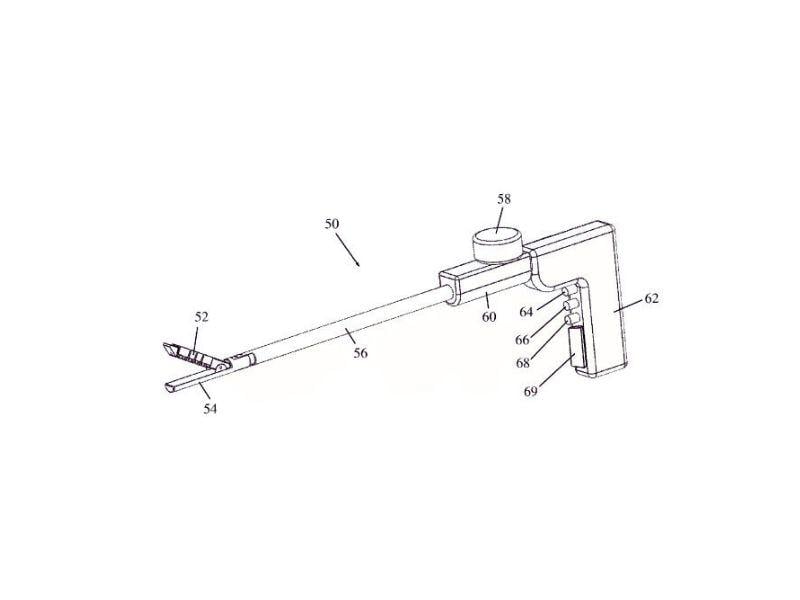
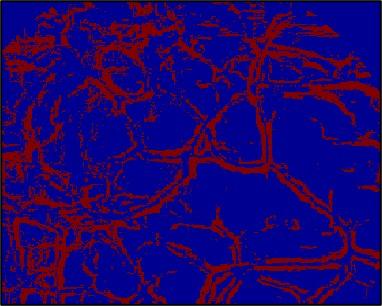
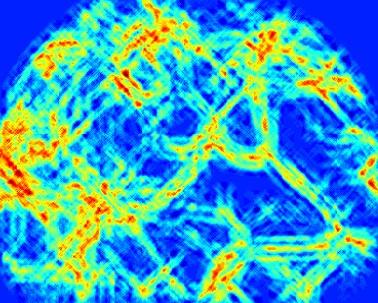
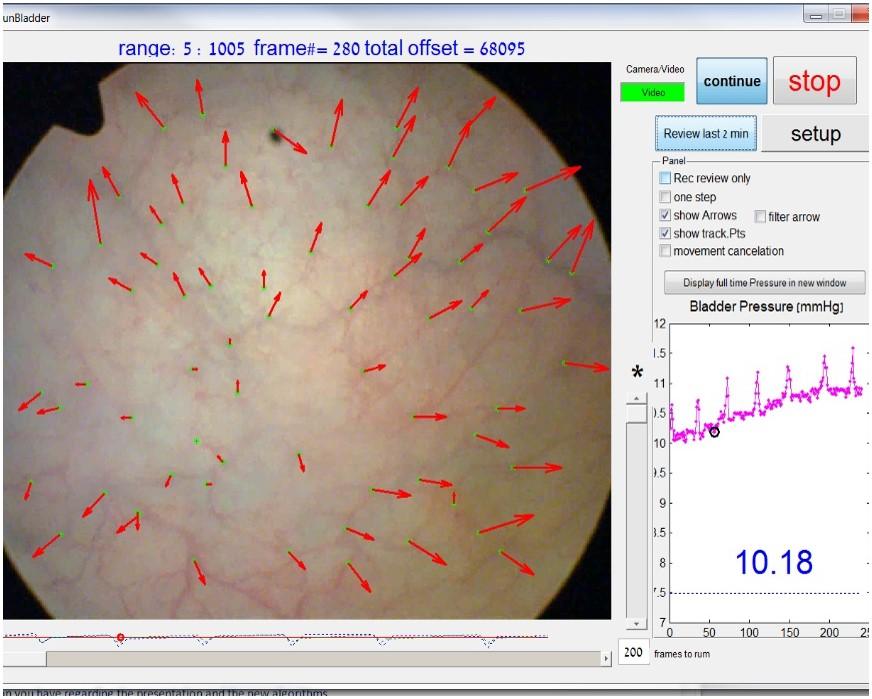
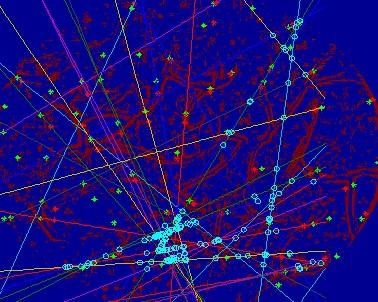
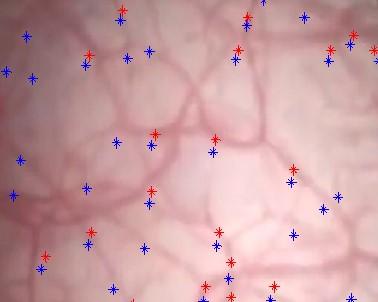
A novel software-based imaging platform was developed to address this need. Integrating seamlessly with standard cystoscopy and pressure-monitoring equipment, the system enables real-time and offline video analysis to guide localized therapy. The platform captures bladder video and pressure data, processes the images to detect vascular bifurcations and contraction patterns, and uses vector analysis to identify focal points of overactivity. These data points are then displayed with graphical overlays, enabling physicians to deliver targeted Botox injections with improved accuracy. Stored video segments and annotated images also support offline review and treatment planning, making follow-up interventions more consistent and effective.
This visual, data-driven approach enables clinicians to focus treatment on the most active zones of the bladder, reducing side effects and enhancing overall therapeutic efficacy.

Development & Validation
Proof-of-concept was demonstrated in a preclinical model, followed by the development of an optimized alpha-stage software capable of capturing and processing both real-time and offline video. The system successfully identified anatomical landmarks and potential sites of overactivity. A more advanced beta version is now under development, with added features for bladder localization and improved clinical workflow.
To verify performance, the software was tested using video recordings from 20 healthy individuals and 20 patients with OAB. Preliminary results indicate that OAB patients show a higher average number of contraction points compared to healthy controls—supporting the tool’s diagnostic potential and clinical relevance.